EMR systems are revolutionizing healthcare, offering streamlined workflows and improved patient care. But navigating the complexities of these systems—from implementation and security to data analytics and future trends—can feel like decoding a medical textbook. This exploration delves into the core functionalities, security protocols, and integration capabilities of EMR systems, offering a practical understanding for anyone interested in this crucial aspect of modern medicine.
Table of Contents
We’ll cover everything from choosing the right vendor and understanding the costs involved to mastering data analytics and ensuring compliance with regulations like HIPAA. We’ll also examine the impact of emerging technologies like AI and machine learning on the future of EMR systems and how they’re shaping the healthcare landscape. Get ready to ditch the paper charts and embrace the digital age of healthcare!
EMR System Features
EMR systems, or Electronic Medical Record systems, are the backbone of modern healthcare, streamlining patient care and administrative tasks. They offer a wide range of features designed to improve efficiency, accuracy, and patient safety. Understanding these features is crucial for choosing the right system for any medical practice.
Core Functionalities of a Typical EMR System
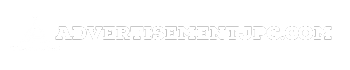
A typical EMR system provides a centralized repository for all patient health information. This includes demographics, medical history, diagnoses, medications, allergies, immunization records, lab results, and imaging reports. Beyond data storage, core functionalities involve appointment scheduling, billing and coding, generating reports, and facilitating secure communication between healthcare providers. Many systems also integrate with other healthcare technologies, such as pharmacy systems and telehealth platforms.
This integration allows for seamless data flow and reduces the potential for errors associated with manual data entry. For example, a lab result can automatically update a patient’s chart, eliminating the need for manual transcription.
Cloud-Based vs. On-Premise EMR Systems
Cloud-based EMR systems store data on remote servers, accessible via the internet. This offers advantages like scalability, accessibility from multiple locations, and reduced IT infrastructure costs. However, reliance on internet connectivity is a potential drawback, and data security concerns require careful consideration. On-premise systems, in contrast, store data on servers located within the medical practice’s own infrastructure.
This provides greater control over data security and eliminates reliance on internet connectivity, but requires significant upfront investment in hardware and IT personnel. A small practice might find the lower initial cost and ease of access of a cloud-based system more appealing, while a large hospital system might prioritize the security and control offered by an on-premise system.
The choice depends heavily on the specific needs and resources of the healthcare provider.
User Interface Design for EMR Systems
A user-friendly interface is paramount for an effective EMR system. The design should prioritize intuitive navigation, clear visual presentation of information, and efficient workflow integration. Imagine a system with a customizable dashboard displaying frequently accessed patient information, a drag-and-drop interface for appointment scheduling, and color-coded alerts for critical patient data, such as allergies or abnormal lab results. The system should also support voice-to-text capabilities for efficient documentation, reducing the time spent on typing and allowing medical professionals to focus on patient interaction.
Templates for common tasks and quick access to relevant information are also essential elements of a well-designed user interface. A clean, uncluttered design with easily identifiable icons and intuitive menus would significantly improve the user experience.
Essential EMR System Features for a Small Medical Practice
For a small medical practice, prioritizing essential features is crucial. The most important features would include a robust patient portal for secure communication and information sharing, integrated billing and scheduling functionalities to streamline administrative tasks, and basic reporting capabilities for tracking key performance indicators. A secure messaging system for communication with patients and other providers is also critical.
While advanced features like sophisticated analytics and telehealth integration are beneficial, they might be less critical initially for a small practice with limited resources. Focusing on core functionalities that directly impact patient care and operational efficiency will be most impactful in the early stages. A phased approach to implementing additional features as the practice grows is a sensible strategy.
EMR System Security
Protecting patient data in electronic medical record (EMR) systems is paramount. A robust security strategy is crucial not only for maintaining patient trust but also for complying with stringent legal and ethical standards. Failure to adequately secure EMR data can lead to significant financial penalties, reputational damage, and, most importantly, harm to patients.EMR System Security MeasuresImplementing comprehensive security measures is essential to safeguard sensitive patient information.
This involves a multi-layered approach encompassing technical, administrative, and physical safeguards. Strong passwords, multi-factor authentication, and regular security audits are fundamental. Encryption of data both in transit and at rest is critical, as is the implementation of access control mechanisms to ensure that only authorized personnel can access specific data. Regular software updates and patching are also vital to address known vulnerabilities.
Finally, a comprehensive employee training program on security best practices is essential to prevent human error, a major source of security breaches.
HIPAA and GDPR Compliance
Compliance with regulations like the Health Insurance Portability and Accountability Act (HIPAA) in the United States and the General Data Protection Regulation (GDPR) in Europe is mandatory for EMR systems. HIPAA dictates specific security rules for protecting Protected Health Information (PHI), including administrative, physical, and technical safeguards. GDPR similarly establishes stringent requirements for data protection, focusing on consent, data minimization, and the right to be forgotten.
Meeting these compliance requirements necessitates rigorous security protocols, regular audits, and demonstrable adherence to best practices. Failure to comply can result in substantial fines and legal repercussions. For example, a hospital failing to adequately secure patient data under HIPAA could face penalties in the hundreds of thousands of dollars per violation.
Potential Vulnerabilities and Mitigation Strategies
EMR systems, like any complex software, are susceptible to various vulnerabilities. Phishing attacks, malware infections, and unauthorized access attempts are common threats. Weak passwords, unpatched software, and insufficient access controls represent significant vulnerabilities. Mitigation strategies include implementing strong password policies, regularly updating software, employing intrusion detection systems, and conducting regular security assessments and penetration testing. Employee training on recognizing and avoiding phishing attempts is also crucial.
Furthermore, robust data loss prevention (DLP) measures can help prevent sensitive data from leaving the system unauthorized. A strong security information and event management (SIEM) system can monitor activity and alert administrators to potential threats in real time.
Hypothetical Security Breach Scenario and Response
Imagine a scenario where an employee clicks a malicious link in a phishing email, resulting in a ransomware attack on the EMR system. The attack encrypts patient data, rendering it inaccessible. The initial response involves isolating the affected system from the network to prevent further spread. Next, a thorough investigation is launched to determine the extent of the breach and identify the source.
This involves analyzing system logs, interviewing staff, and collaborating with cybersecurity experts. Data recovery efforts begin, potentially involving restoring data from backups. Finally, a notification process is initiated, informing affected patients and regulatory bodies as required by HIPAA and other relevant regulations. Lessons learned from the incident are then used to improve security protocols and prevent future breaches.
This might involve strengthening password policies, implementing multi-factor authentication across the board, and conducting more frequent security awareness training.
EMR System Integration
EMR systems don’t exist in a vacuum; their true power comes from their ability to connect and share data with other healthcare IT systems. Seamless integration is crucial for improving patient care, streamlining workflows, and reducing the risk of errors. This section explores how EMRs integrate with other systems, highlighting successful examples, common challenges, and solutions.EMR systems integrate with various other healthcare IT systems through a variety of methods, including HL7 (Health Level Seven) messaging, APIs (Application Programming Interfaces), and direct database connections.
The specific integration method depends on the systems involved and the data being exchanged. Commonly integrated systems include Hospital Information Systems (HIS), Laboratory Information Systems (LIS), Pharmacy Information Systems (PIS), Radiology Information Systems (RIS), and billing systems. The goal is to create a unified view of the patient’s health record, accessible to all relevant healthcare providers.
Integration with Other Healthcare IT Systems
EMR systems achieve integration with other systems like HIS, LIS, and PIS primarily through standardized data exchange protocols. HL7, for instance, provides a framework for exchanging clinical data between different systems, ensuring interoperability. APIs allow for more customized and dynamic data exchange, enabling real-time updates and integration with specialized applications. Database connections, while offering high speed, often require more significant development effort and pose greater security concerns.
Successful integration requires careful planning, thorough testing, and ongoing maintenance.
Examples of Successful EMR System Integrations and Achieved Benefits
The integration of Epic EMR with Cerner Millennium HIS in a large hospital system resulted in a significant reduction in medication errors and improved patient safety. By sharing real-time medication information between the two systems, pharmacists could identify potential drug interactions and alert clinicians before prescriptions were administered. This streamlined workflow also reduced administrative burden and improved overall efficiency.
Another example is the integration of an EMR with a LIS, which allows lab results to be automatically populated into the patient’s chart, eliminating manual data entry and reducing the risk of transcription errors. This leads to faster diagnosis and treatment.
Challenges Encountered During EMR System Integration Projects and Their Solutions
One significant challenge is data standardization. Different systems may use different data formats and terminologies, making it difficult to exchange information seamlessly. Solutions include using standardized vocabularies like SNOMED CT and LOINC, and employing data mapping techniques to translate data between different formats. Another challenge is ensuring data security and privacy. Integrating systems requires careful consideration of access controls and data encryption to protect sensitive patient information.
Implementing robust security measures, including role-based access control and audit trails, is crucial. Finally, budget constraints and limited technical expertise can hinder successful integration. Careful planning, phased implementation, and collaboration with experienced IT professionals can help mitigate these challenges.
Workflow Demonstrating Seamless Data Exchange Between an EMR System and a Pharmacy System
A patient’s physician enters a prescription for a medication within the EMR system. The EMR system, using an API, sends the prescription details (patient demographics, medication details, dosage, etc.) electronically to the pharmacy system. The pharmacy system verifies the prescription against the patient’s insurance information and checks for potential drug interactions. The pharmacist reviews the prescription and, upon approval, dispenses the medication.
The pharmacy system then sends a confirmation message back to the EMR system, updating the patient’s medication list. This seamless data exchange ensures accuracy, reduces errors, and improves patient safety. If there are any issues with the prescription, an alert is sent back to the physician through the EMR system, facilitating timely intervention.
EMR System Implementation
Implementing a new Electronic Medical Record (EMR) system is a significant undertaking for any healthcare organization, requiring careful planning, execution, and ongoing support. A successful implementation hinges on a well-defined strategy that addresses technological, logistical, and human factors. This process can be complex and challenging, but with meticulous preparation and a dedicated team, the transition can be smooth and ultimately beneficial.
The implementation process generally involves several key phases, each with its own set of tasks and potential challenges. These phases often overlap and require constant communication and collaboration among various stakeholders, including clinicians, IT staff, administrators, and vendors.
EMR System Implementation Steps
Implementing a new EMR system requires a systematic approach. A typical implementation follows these steps: Needs Assessment and Planning, System Selection, Vendor Contract Negotiation, Data Migration, System Configuration and Customization, Training and Education, Go-Live and Post-Implementation Support. Each of these steps involves numerous sub-tasks and requires significant resources. For example, the needs assessment phase requires detailed analysis of current workflows and identification of future needs.
System selection involves evaluating various vendors and systems based on the organization’s specific requirements.
Potential Challenges and Risks Associated with EMR System Implementation
Several challenges and risks can hinder a successful EMR implementation. These include inadequate planning, insufficient budget allocation, resistance from healthcare professionals to adopting new technology, data migration issues, integration difficulties with existing systems, and inadequate training. For example, insufficient training can lead to user errors and decreased efficiency, while integration problems can disrupt workflows and compromise data integrity.
Poorly managed data migration can result in data loss or inaccuracies, impacting the reliability of patient information.
EMR System Implementation Checklist
A comprehensive checklist is essential for successful EMR implementation. This checklist should cover all phases of the implementation, from initial planning to post-implementation support. Key areas to include are: defining project scope and objectives, securing necessary funding and resources, establishing a project timeline and milestones, developing a communication plan, selecting and configuring the EMR system, performing data migration and validation, providing comprehensive training to all users, establishing a robust support system, and creating a post-implementation review process.
Each item on the checklist should be assigned to a specific team member and include a target completion date.
Timeline for Implementing an EMR System in a Large Hospital
Implementing an EMR system in a large hospital is a complex project requiring a detailed timeline. The following is a sample timeline, which should be adjusted based on the specific needs and resources of the organization.
| Phase | Milestone | Deliverable | Timeline (Months) |
|---|---|---|---|
| Needs Assessment & Planning | Complete needs assessment | Needs assessment report | 1-2 |
| System Selection | Select EMR vendor | Vendor contract | 2-3 |
| Data Migration | Migrate patient data | Migrated data validation report | 3-4 |
| System Configuration & Customization | Configure and customize the system | Configured system | 2-3 |
| Training & Education | Train all users | Training completion reports | 1-2 |
| Go-Live & Post-Implementation Support | Go-live with the new EMR system | Go-live report | 1+ |
EMR System Cost and ROI
Choosing an EMR system is a big financial decision for any healthcare practice. It’s not just about the initial purchase price; the long-term costs and the return on that investment need careful consideration. Understanding the various cost components and how to calculate ROI is crucial for making an informed choice.The total cost of ownership (TCO) for an EMR system goes far beyond the initial software license fee.
Many factors contribute to the overall expense, making accurate budgeting essential.
EMR System Cost Components
Several key cost factors influence the overall expense of implementing and maintaining an EMR system. These include software licensing fees (which can vary based on the number of users and modules), hardware costs (servers, workstations, and peripherals), implementation costs (consultant fees, training, data migration), ongoing maintenance and support fees (software updates, technical support), and staff training costs (initial and ongoing training for clinicians and administrative staff).
Hidden costs, such as potential downtime during implementation and the cost of addressing unforeseen technical issues, should also be factored in. For example, a small clinic might spend $10,000 on software licenses, $5,000 on hardware, and $15,000 on implementation, while a larger hospital could easily spend hundreds of thousands, if not millions, depending on the scale and complexity of the system.
Total Cost of Ownership (TCO) Comparison Across Vendors
Direct comparison of TCO across different EMR vendors is difficult due to variations in pricing models, features, and support levels. Some vendors offer subscription-based models, while others use a one-time purchase model. Furthermore, the complexity of the system and the level of customization required significantly impact the overall cost. For example, a cloud-based EMR system might have lower upfront costs but higher ongoing subscription fees compared to an on-premise system with a higher initial investment but potentially lower long-term maintenance costs.
To compare effectively, potential buyers need to obtain detailed quotes from multiple vendors, carefully comparing features and support services included in each package. They should also consider hidden costs and potential future upgrades.
Return on Investment (ROI) Calculation for EMR Systems
Calculating the ROI for an EMR system involves comparing the total cost of ownership (TCO) with the quantifiable benefits achieved. A simple ROI calculation can be expressed as:
ROI = (Net Benefits – Total Costs) / Total Costs
To determine net benefits, healthcare providers need to identify and quantify the improvements resulting from EMR adoption.
Quantifiable Benefits Justifying EMR Investment
Implementing an EMR system offers several quantifiable benefits that can significantly improve efficiency and profitability. These include increased billing accuracy and reduced claim denials, leading to improved revenue cycle management. Improved patient care coordination, reduced medical errors, and enhanced patient satisfaction are other benefits. For instance, a reduction in medication errors could lead to significant cost savings by preventing hospital readmissions and associated expenses.
Similarly, streamlined billing processes can reduce administrative overhead and free up staff time for patient care. A study by the American Academy of Family Physicians showed that EMR adoption led to a 15% increase in efficiency for physicians, allowing them to see more patients and generate more revenue. This increase in efficiency, coupled with a reduction in billing errors, directly contributes to a positive ROI.
EMR System Training and Support
Successfully implementing an EMR system hinges not just on its technical capabilities, but also on the effectiveness of its training and ongoing support. A well-structured training program empowers medical staff to confidently utilize the system, maximizing its benefits and minimizing disruptions to workflow. Equally crucial is continuous support to address evolving needs and troubleshoot any arising issues.A comprehensive EMR system training program needs to be multifaceted, addressing the varying needs and skill levels of different medical professionals.
It shouldn’t be a one-size-fits-all approach; rather, it should be tailored to specific roles and responsibilities within the healthcare setting. This ensures that training is both efficient and effective, leading to faster adoption and improved user satisfaction.
Components of a Comprehensive EMR System Training Program
Effective EMR training involves a blended learning approach. This combines instructor-led sessions, hands-on practice with the system in a simulated environment, and readily accessible online resources for continued learning and reference. The curriculum should cover all essential system modules, focusing on practical application and real-world scenarios.
- Needs Assessment: Before designing the training program, a thorough needs assessment should be conducted to identify the specific training requirements of different user groups (physicians, nurses, administrative staff, etc.).
- Instructor-Led Training: Interactive sessions led by experienced trainers who can answer questions and provide personalized guidance. These sessions should focus on key functionalities and common workflows.
- Hands-on Practice: Dedicated time for practical application of learned skills using a simulated EMR environment. This allows users to practice without impacting real patient data.
- Online Resources: A comprehensive online portal with tutorials, FAQs, videos, and troubleshooting guides. This provides readily accessible support after the initial training period.
- Super User Program: Identifying and training key personnel within each department to act as internal experts and provide peer-to-peer support.
- Ongoing Assessments and Feedback: Regular assessments to gauge user understanding and identify areas needing further attention. Feedback mechanisms allow for continuous improvement of the training program.
Importance of Ongoing Support and Maintenance
Ongoing support extends beyond the initial training phase. It is crucial for addressing technical issues, providing updates on system enhancements, and ensuring the system remains optimized for peak performance. Proactive maintenance minimizes downtime and prevents potential problems from escalating. This also includes regular software updates, security patches, and hardware maintenance to ensure data integrity and system reliability.
Without this, the system’s efficiency and user satisfaction can drastically decline. For example, a hospital experiencing frequent EMR crashes due to lack of maintenance might see a significant drop in productivity and an increase in errors.
Key Performance Indicators (KPIs) for EMR System Training Success
Measuring the effectiveness of EMR system training requires the use of specific KPIs. These metrics provide insights into user proficiency, system adoption rates, and overall training program efficacy. Tracking these KPIs allows for continuous improvement and ensures that the training program is meeting its objectives.
- User Proficiency: Measured through assessments and observed performance during hands-on practice. This can include timed tasks or scenario-based evaluations.
- System Adoption Rate: The percentage of staff actively using the EMR system for their daily tasks. This reflects the overall success of the training in getting users to embrace the new technology.
- Training Completion Rate: The percentage of staff who successfully complete the training program. This indicates the effectiveness of the training delivery methods and the accessibility of the resources.
- User Satisfaction: Gathered through surveys and feedback sessions to understand user experiences and identify areas for improvement.
- Error Rate: Tracking the number of errors made while using the EMR system. A decrease in errors indicates improved user proficiency and system understanding.
Sample Training Manual: Medication Ordering Module
This section provides a simplified example of a training manual excerpt focusing on the medication ordering module of a hypothetical EMR system, “MediChart.” MediChart Medication Ordering Module: Training Manual ExcerptObjective: To learn how to safely and efficiently order medications using the MediChart EMR system. Module Overview: This module covers the process of medication ordering, from selecting the appropriate medication to verifying the order before submission. Step-by-Step Instructions:
1. Patient Selection
Locate the patient’s chart by searching using their name, medical record number, or date of birth.
2. Medication Search
Use the search function to find the desired medication. The system utilizes both generic and brand names. Be sure to select the correct dosage form and strength.
3. Order Entry
Enter the prescribed dose, frequency, route of administration, and duration. The system will provide warnings for potential drug interactions or allergies.
4. Order Review
Carefully review all entered information before submitting the order. Verify patient details, medication details, and dosage instructions.
5. Order Submission
Once you’ve reviewed the order, click “Submit Order.” The system will generate a confirmation message and record the order in the patient’s chart. Troubleshooting: If you encounter any errors during the medication ordering process, refer to the online troubleshooting guide or contact the IT support team.
EMR System Data Analytics
EMR systems are more than just digital repositories of patient information; they’re powerful tools for generating data-driven insights that can significantly improve both patient care and operational efficiency. By leveraging the vast amounts of data contained within these systems, healthcare providers can identify trends, predict outcomes, and make more informed decisions, ultimately leading to better health outcomes and cost savings.
This section explores how EMR data analytics can be harnessed for these purposes.EMR data can be used to improve patient care and operational efficiency in numerous ways. For instance, analyzing patient data can help identify high-risk individuals who might benefit from preventative care or more intensive monitoring. Operational efficiency gains can be achieved through identifying bottlenecks in workflows, optimizing staffing levels, and improving resource allocation.
The ability to track key performance indicators (KPIs) provides valuable insights into areas needing improvement.
Data-Driven Insights from EMR Systems
EMR systems offer a wealth of data that can be analyzed to reveal actionable insights. For example, analyzing medication adherence data can identify patients at risk of non-compliance, allowing for timely interventions. Similarly, analyzing readmission rates can highlight areas where care could be improved to reduce hospital readmissions. Predictive modeling, using historical data, can help predict future patient needs and optimize resource allocation.
Identifying patterns in patient demographics and diagnoses can help tailor services and improve patient outcomes. For example, a hospital might discover that a specific demographic is more likely to experience a particular complication after surgery, leading to preventative measures for that group.
Data Governance and Data Quality Management
Effective data governance and quality management are crucial for ensuring the reliability and validity of data-driven insights. This involves establishing clear policies and procedures for data collection, storage, and access. Data quality checks should be regularly implemented to identify and correct errors or inconsistencies. Data security measures must be in place to protect patient privacy and comply with regulations such as HIPAA.
EMR systems are crucial for healthcare providers, managing patient data and billing. But managing the financial side of things can be a whole other beast, which is where software like intuit quickbooks comes in handy for tracking revenue and expenses. Ultimately, smooth financial operations are just as important as efficient EMR systems for a successful practice.
Regular audits and data validation processes are essential for maintaining data integrity and ensuring the accuracy of analyses. Furthermore, establishing a data governance team with clear responsibilities and accountability can help to streamline these processes.
EMR System Dashboard Design
The following table Artikels a sample dashboard design visualizing key metrics extracted from an EMR system. This dashboard focuses on providing a high-level overview of key performance indicators related to patient care and operational efficiency.
| Metric | Value | Trend | Target |
|---|---|---|---|
| Average Length of Stay (LOS) | 3.2 days | Decreasing | 3.0 days |
| Readmission Rate (within 30 days) | 5% | Increasing | 4% |
| Patient Satisfaction Score | 4.5/5 | Stable | 4.7/5 |
| Medication Adherence Rate | 88% | Decreasing | 90% |
| Number of Emergency Room Visits | 120 per month | Increasing | 100 per month |
| Average Wait Time (Appointments) | 15 minutes | Decreasing | 10 minutes |
EMR System Usability and Workflow
EMR systems are crucial for modern healthcare, but their effectiveness hinges heavily on usability. A poorly designed system can significantly hinder physician workflow, leading to decreased efficiency, increased burnout, and ultimately, reduced patient satisfaction. Conversely, a user-friendly EMR can streamline processes, improve accuracy, and enhance the overall patient experience. This section explores the intricate relationship between EMR usability, workflow optimization, and the impact on both clinicians and patients.
The impact of EMR usability on physician workflow and patient satisfaction is multifaceted. A clunky, time-consuming system forces doctors to spend more time on data entry and less time with patients, leading to frustration and potential medical errors. This translates directly to lower patient satisfaction as patients feel rushed or neglected. Conversely, an intuitive system allows physicians to quickly access necessary information, document efficiently, and dedicate more time to direct patient care.
This results in improved patient-physician interaction and increased patient satisfaction scores. Studies have shown a strong correlation between EMR usability and physician job satisfaction, highlighting the importance of investing in user-friendly systems.
Common Usability Issues and Proposed Solutions
Poorly designed EMR systems often present significant usability challenges. These challenges frequently stem from issues with navigation, data entry, and overall system design. For example, complex search functions, poorly organized menus, and inconsistent data entry requirements can drastically slow down workflow.
To address these issues, several solutions can be implemented. These include: improving search functionality with intuitive filters and autocomplete features; simplifying navigation through clear visual cues and logical menu structures; standardizing data entry fields and formats across the system; providing contextual help and training resources within the EMR interface; and prioritizing the development of customizable user profiles to accommodate individual physician preferences.
Regular feedback mechanisms, including user surveys and focus groups, can further identify and address usability concerns.
Comparison of EMR User Interfaces
Let’s consider two hypothetical EMR systems: System A and System B. System A boasts a traditional, menu-driven interface with numerous nested menus and a complex search function. Data entry often requires multiple clicks and scrolling through extensive lists. System B, on the other hand, employs a more modern, intuitive design. It utilizes a drag-and-drop interface for certain tasks, a powerful search bar with predictive text, and color-coded alerts for critical information.
The effectiveness of these interfaces is starkly different. System A’s complexity leads to increased time spent on data entry and a higher likelihood of errors. Physicians using System A often report frustration and decreased efficiency. System B’s streamlined design, however, fosters a more efficient workflow, reducing the time required for documentation and improving overall physician satisfaction. The intuitive interface also minimizes errors and promotes a smoother patient interaction.
This difference underscores the importance of investing in user-centered design when selecting or developing an EMR system.
Workflow Optimization Strategy for Reduced Data Entry Time
A key strategy for optimizing workflow and reducing data entry time involves leveraging features like templating, macros, and voice recognition.
Templating allows physicians to create pre-populated forms for common procedures or patient encounters, significantly reducing repetitive data entry. Macros automate frequently performed tasks, such as generating prescriptions or referral letters. Voice recognition software enables physicians to dictate clinical notes, freeing up their hands and speeding up the documentation process. Additionally, implementing data integration with other systems, such as laboratory information systems (LIS) and pharmacy systems, can eliminate the need for manual data entry of test results and medication information.
Finally, regular training and ongoing support for staff are crucial to ensure that these tools are used effectively and efficiently.
EMR System Interoperability

Interoperability in electronic health record (EHR) systems, often shortened to EMR, is the ability of different systems to exchange and use information seamlessly. This means that data from one EMR system can be easily accessed and understood by another, regardless of the vendor or technology used. It’s crucial for improving patient care, reducing medical errors, and streamlining healthcare workflows.EMR interoperability is not just about transferring data; it’s about ensuring that the data is correctly interpreted and utilized by the receiving system.
Without interoperability, healthcare providers may struggle to access a complete patient record, leading to potential delays in treatment and duplicated testing. This is particularly important in situations involving multiple specialists or hospitals.
Benefits of EMR System Interoperability
Achieving interoperability offers significant advantages. Improved patient care is paramount, as clinicians have access to a more complete picture of the patient’s health history, leading to better-informed decisions. This reduces the risk of medication errors and adverse events due to incomplete or conflicting information. Furthermore, streamlined workflows increase efficiency and reduce administrative burdens, freeing up staff to focus on patient care.
Finally, cost savings can be achieved through reduced duplication of services and improved coordination of care.
Challenges of Achieving EMR System Interoperability
Despite the benefits, achieving interoperability presents considerable hurdles. Different EMR systems use various data formats and communication protocols, creating compatibility issues. Data security and privacy concerns are also significant, as the exchange of sensitive patient information requires robust security measures. The cost of implementing and maintaining interoperability solutions can be substantial, particularly for smaller healthcare providers. Furthermore, a lack of standardized data formats and interoperability protocols has historically hampered progress.
Finally, the integration of legacy systems into a unified interoperable network presents a significant technological challenge.
Standards and Technologies Supporting EMR System Interoperability
Several standards and technologies are driving progress in EMR interoperability. The Fast Healthcare Interoperability Resources (FHIR) standard, developed by HL7 (Health Level Seven International), is gaining widespread adoption. FHIR uses RESTful APIs, making it easier to integrate different systems. Other important standards include HL7 v2 and v3, although FHIR is generally considered more flexible and modern. These standards define the structure and content of healthcare data, facilitating seamless exchange between systems.
DICOM (Digital Imaging and Communications in Medicine) is another key standard, specifically for medical imaging data.
Data Exchange Between Different EMR Systems
Imagine two hospitals, Hospital A and Hospital B, using different EMR systems. They need to exchange a patient’s allergy information. * Step 1: Hospital A’s EMR system packages the patient’s allergy information according to the FHIR standard.
Step 2
The data is sent securely over a network using a standard communication protocol (e.g., HTTPS).
Step 3
Hospital B’s EMR system receives the data and validates its authenticity and integrity.
Step 4
Hospital B’s EMR system parses the FHIR message and integrates the allergy information into the patient’s record.
EMR System Vendor Selection
Choosing the right EMR vendor is a critical decision for any healthcare organization. A poorly chosen system can lead to workflow disruptions, decreased efficiency, and ultimately, negatively impact patient care. The selection process requires careful consideration of various factors, from the vendor’s reputation and financial stability to the system’s functionality and integration capabilities. A thorough evaluation will ensure a smooth implementation and maximize the return on investment.
Criteria for Selecting an EMR System Vendor
Several key criteria should guide the vendor selection process. These criteria can be broadly categorized into functional requirements, technical capabilities, vendor support, and financial considerations. A weighted scoring system can be used to objectively compare different vendors based on the importance of each criterion.
- Functionality: Does the system meet the specific needs of the practice or hospital? This includes features like appointment scheduling, electronic prescribing, patient portals, and clinical documentation tools. Consider the specific needs of different departments or specialties.
- Interoperability: Can the system seamlessly integrate with existing systems, such as laboratory information systems (LIS) and radiology information systems (RIS)? This is crucial for avoiding data silos and ensuring a holistic view of patient information.
- Usability and Workflow: Is the system intuitive and easy to use for all staff members? A user-friendly interface can significantly improve efficiency and reduce training time.
- Security: Does the vendor have robust security measures in place to protect patient data? Compliance with HIPAA regulations is essential.
- Vendor Support: What level of support does the vendor provide? This includes technical support, training, and ongoing maintenance. Consider the vendor’s reputation for responsiveness and expertise.
- Cost and ROI: What is the total cost of ownership, including software licensing, hardware, implementation, training, and ongoing maintenance? Can the vendor demonstrate a clear return on investment?
Comparison of Three EMR System Vendors
Let’s compare three hypothetical vendors: Meditech, Epic, and Cerner. These are not real-world comparisons but serve as illustrative examples.
| Criterion | Meditech | Epic | Cerner |
|---|---|---|---|
| Functionality | Comprehensive, customizable | Highly specialized, extensive features | Broad range of functionalities, strong in hospital settings |
| Interoperability | Good integration capabilities | Excellent interoperability, known for robust HL7 interfaces | Strong integration capabilities, extensive API support |
| Usability | Moderate learning curve | Steep learning curve, highly specialized | Moderate learning curve, user-friendly interface |
| Security | Strong security features, HIPAA compliant | Robust security, high level of data protection | Excellent security protocols, certified for HIPAA compliance |
| Vendor Support | Responsive support team, extensive documentation | Extensive support network, but can be costly | Good support, proactive maintenance |
| Cost | Moderate | High | High |
Request for Proposal (RFP) Document for an EMR System
The RFP should clearly Artikel the organization’s requirements, including functional specifications, technical requirements, implementation timelines, and budget constraints. It should also include a detailed evaluation criteria and a process for vendor selection.
- Introduction: Briefly describe the organization and its needs.
- Background: Explain the reasons for seeking a new EMR system.
- Requirements: Detail the functional and technical requirements of the system.
- Implementation Plan: Artikel the desired implementation timeline and process.
- Evaluation Criteria: Specify the criteria that will be used to evaluate vendor proposals.
- Submission Instructions: Provide clear instructions on how to submit proposals.
Decision Matrix for Evaluating EMR System Vendors
A decision matrix provides a structured approach to comparing different vendors based on pre-defined criteria. Each criterion is assigned a weight reflecting its importance, and each vendor is scored based on its performance in each area. The weighted scores are then summed to provide an overall score for each vendor.
| Criterion | Weight | Vendor A | Vendor B | Vendor C |
|---|---|---|---|---|
| Functionality | 30% | 8 | 7 | 9 |
| Interoperability | 20% | 7 | 9 | 8 |
| Usability | 20% | 6 | 5 | 7 |
| Security | 15% | 9 | 8 | 9 |
| Vendor Support | 10% | 7 | 6 | 8 |
| Cost | 5% | 6 | 4 | 5 |
| Weighted Score | 7.25 | 6.85 | 7.95 |
Future Trends in EMR Systems
The healthcare landscape is undergoing a rapid transformation, driven by technological advancements and a growing emphasis on data-driven decision-making. EMR systems are at the forefront of this change, evolving from simple record-keeping tools to sophisticated platforms integrating advanced technologies that promise to revolutionize patient care and healthcare operations. This section explores the emerging trends shaping the future of EMR systems.
Artificial Intelligence and Machine Learning in EMRs
AI and machine learning (ML) are poised to significantly impact EMR systems. These technologies can analyze vast amounts of patient data to identify patterns, predict health risks, personalize treatment plans, and automate administrative tasks. For example, AI algorithms can analyze patient data to predict the likelihood of readmission, allowing healthcare providers to proactively intervene and improve patient outcomes. ML models can personalize medication dosages based on individual patient characteristics and response to treatment.
The integration of AI and ML promises to enhance the efficiency and effectiveness of healthcare delivery, leading to better patient care and reduced costs. However, challenges remain, including data privacy concerns, the need for robust validation of AI algorithms, and the potential for algorithmic bias.
The Rise of Cloud-Based EMR Systems
Cloud computing offers significant advantages for EMR systems, including scalability, accessibility, and cost-effectiveness. Cloud-based EMRs allow healthcare providers to access patient data from anywhere with an internet connection, improving collaboration and care coordination. Furthermore, cloud platforms offer enhanced security features and automatic backups, reducing the risk of data loss. The scalability of cloud-based systems allows healthcare organizations to easily adapt to changing needs, accommodating growth and fluctuations in patient volume.
However, concerns regarding data security and vendor lock-in remain important considerations when adopting cloud-based EMR solutions. For instance, the transition to a cloud-based system for a large hospital network requires careful planning and significant investment in data migration and staff training.
Interoperability and Data Exchange, Emr systems
Enhanced interoperability between different EMR systems and other healthcare IT systems is crucial for seamless information exchange. This allows for better care coordination across different healthcare settings and providers. Standardized data formats and APIs are essential for achieving true interoperability. Imagine a scenario where a patient’s complete medical history, including lab results, imaging reports, and medication records, is readily available to any healthcare provider involved in their care, regardless of the EMR system used.
This improved data exchange fosters better informed decision-making and enhances the quality of patient care. However, achieving widespread interoperability requires overcoming challenges related to data standardization, security, and regulatory compliance.
Personalized Medicine and Precision Healthcare
EMR systems are playing an increasingly important role in supporting personalized medicine initiatives. By integrating genomic data, lifestyle information, and other relevant factors, EMRs can help tailor treatment plans to individual patient needs. For example, an EMR system could identify patients at high risk for certain diseases based on their genetic profile, allowing for early intervention and preventive measures.
This approach to healthcare promises to improve treatment outcomes and reduce healthcare costs by focusing resources on the most effective interventions for each patient. The successful implementation of personalized medicine requires robust data integration capabilities within the EMR system and the development of algorithms capable of analyzing complex patient data.
A Conceptual Model for a Future-Generation EMR System
A future-generation EMR system would seamlessly integrate AI, ML, cloud computing, and advanced interoperability features. It would be a highly personalized, patient-centric platform, providing a comprehensive view of each patient’s health journey. This system would leverage predictive analytics to identify potential health risks, automate administrative tasks, and facilitate proactive interventions. Data security and privacy would be paramount, incorporating robust encryption and access control mechanisms.
The system would also support seamless integration with wearable devices and other telehealth technologies, providing real-time data to healthcare providers. The user interface would be intuitive and user-friendly, designed to streamline workflows and enhance the overall user experience for both clinicians and patients. This system would represent a significant advancement in healthcare technology, leading to more efficient, effective, and personalized care.
Closing Summary
From initial implementation hurdles to the long-term benefits of improved patient care and operational efficiency, EMR systems present both challenges and immense opportunities. Understanding the intricacies of security, integration, and data analytics is crucial for maximizing their potential. As technology continues to evolve, so too will EMR systems, promising even more sophisticated tools and enhanced capabilities to revolutionize healthcare delivery.
So buckle up, it’s going to be an exciting ride!
Answers to Common Questions: Emr Systems
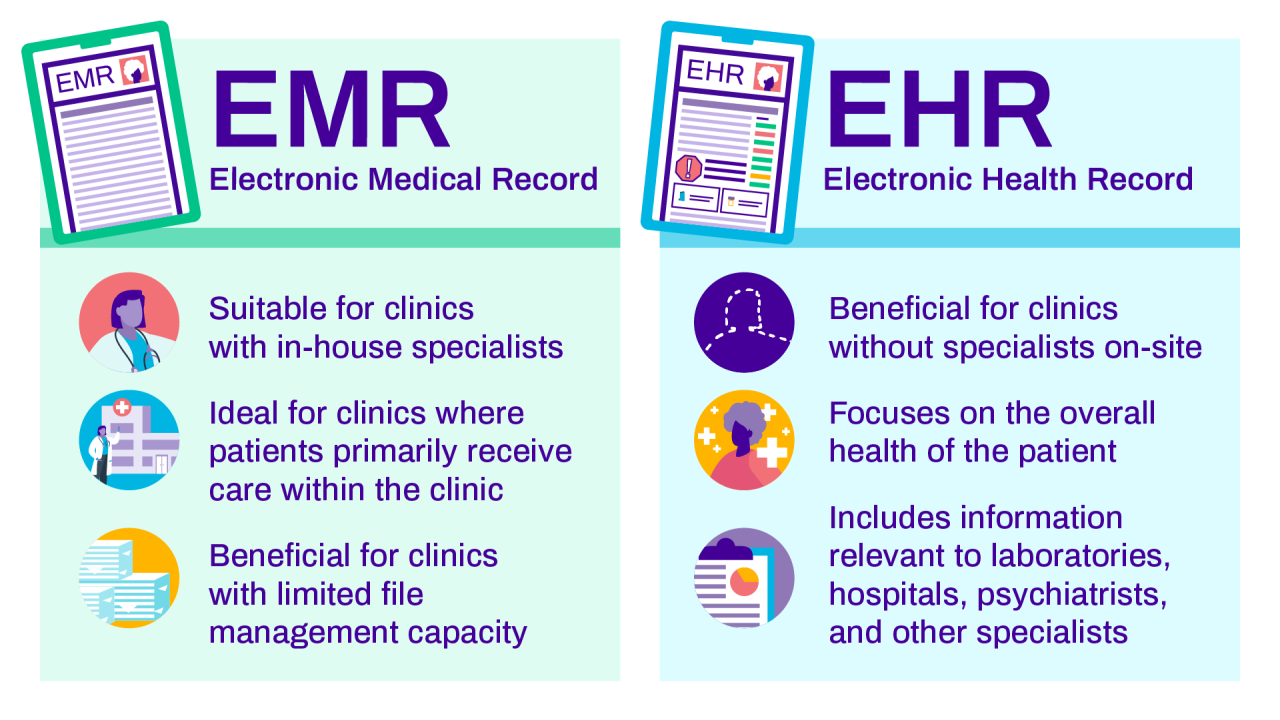
What’s the difference between an EMR and an EHR?
While often used interchangeably, EMR (Electronic Medical Record) focuses on a single practice’s data, while EHR (Electronic Health Record) offers a broader, more comprehensive view of a patient’s health history across multiple providers.
How much does an EMR system cost?
Costs vary wildly depending on the size of your practice, the vendor, and the features included. Expect to pay anywhere from a few thousand dollars annually for smaller practices to hundreds of thousands for larger hospitals, factoring in software licenses, hardware, implementation, training, and ongoing support.
Are EMR systems user-friendly?
User-friendliness is a major concern. Some systems are notoriously clunky and time-consuming to navigate, leading to physician burnout. However, many vendors are prioritizing intuitive design and workflow optimization to address this.
What about data privacy and security breaches?
Patient data is incredibly sensitive. Robust security measures, including encryption, access controls, and regular audits, are critical. Compliance with HIPAA and other regulations is non-negotiable. A breach can have serious legal and financial consequences.
Can EMR systems integrate with my existing software?
Ideally, yes. Seamless integration with other healthcare IT systems (like billing software, labs, and pharmacies) is a major advantage, streamlining workflows and preventing data silos. However, integration can be challenging and may require specialized expertise.